Right now the thing on my mind is catecholamines. I just did a 24-hour urine study to check my catecholamine levels. So, I've been trying to understand them.
As part of our ability to survive as a species, the human body needs to be able to change internal things from one minute to the next, rather quickly and without our involvement, and regardless of what is happening in the environment outside the body, but also in response to it.
Changes in temperature, the humidity, and barometer or any danger we may find ourselves in, require the body to react quickly in order to maintain homeostasis (the body being in a stable state, normal operation). The hypothalamus does this through the Autonomic Nervous System and the endocrine glands.
The Autonomic Nervous System or ANS is one of the systems in our body that responds to changes in position. Around 25% to 30% of our blood volume is in the upper chest when we are laying down. But when we stand up between 300 and 800 mL of the blood moves to the lower body and extremities, helped along by gravity. This is a 25% to 30% drop in volume. Half of this happens during the first few minutes after we stand up.This causes a drop in the blood flow going back to the heart. That in turn, cause a drop in arterial pressure.
In order for you to remain standing and maintain adequate blood flow to the brain, several systems in your body have to be regulated.One of which is your blood pressure. Your blood pressure as to stabilize within about a minute after you stand up.
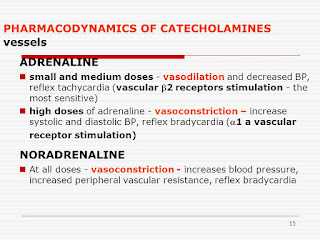
In Hyperadrenergic POTS, there is an abnormally large increase in plasma norepinephrine and a RISE of blood pressure instead of a drop when you stand up. The criteria for Hyperadrenergic POTS is an increase in systolic blood pressure >10 mmHg during 10 minutes of head-up tilt(HUT), as well as an increase of plasma norepinephrine, >600 pg/mL.
Patients usually have a rise in heart rate like other POTS patients, but also have symptoms like palpitations,anxiety, tachycardia and tremulousness. When a ganglionic blockade called trimethaphan is administered, they have a larger drop in BP than other patients, and their upright plasma norepinephrine levels are higher than non-hyperadrenergic POTS patients. When upright, individuals may experience a sense of anxiety, tremor, and cold sweaty hands and feet. Also, in a good portion of individuals, there is a significant urge to pass urine after even a short period of time upright (I wonder if this is why I have to run to the bathroom as soon as I stand up?). True migraine headaches are also common.
NMH or Orthostatic Tachycardia is most likely to occur if you have a
decrease in norepinephrine and an
increase in epinephrine. POTS is the opposite, it is most likely to result from an
increase in norepinephrine and a
decrease in epinephrine.
An interesting article I read on Medscape.com said that people with Hyperadrenergic POTS have exaggerated pressor and sometimes tachycardia response to both orthostatic and other types of stress. It said it's important for them to minimize the reduction of blood flow back to the heart and pulse pressure. This can be helped by volume expansion, i.e. staying hydrated, and wearing an abdominal binder, which reduces vein capacity. Physical counter-maneuvers help too. Counter maneuvers are when you contract certain muscles in order to help blood flow back to the heart.
One really interesting thing the article said was that Inderal(propranolol0, which is a non-β-selective lipophilic agent, at about 10mg a day may work better than atenolol, which is a β-selective lipophilic agent. I happen to be on atenolol right now. Some people have such high BP jumps when they stand, (as much as 250/150 mmHg), that they have to be given phenobarbital. Sometimes they are helped
by clonidine or drugs in the same class.
I found the following on a
Vanderbilt University website: "Some studies have labeled patients with “Hyperadrenergic POTS” if the patient’s upright plasma norepinephrine level is >600 pg/ml. Other studies label patients with “Neuropathic POTS”if the QSART sweat test is abnormal. Someone in the first study might say “I have hyperadrenergic POTS”, while the person in the second study might say “I have neuropathic POTS”. The truth is that at least some (if not many) of those patients will have both abnormalities. Often, these terms are not used to describe mutually exclusive subtypes, but to describe specific findings."
One related condition is pheochromocytoma (a norepinephrine producing tumor) and tests may be needed to differentiate between pheochromocytoma and hyperadrenergic POTS.
Another condition that is similar to Hyperadrenergic POTS is Norepinephrine Transporter (NET) Deficiency. It is thought to be an abnormality in a gene that leads to too much norepinephrine circulating in the body. It can be treated with a class of antidepressants called SNRIs, which will block these transporters. However, some people experience an increase in HR and can't take them.
Inappropriate sinus tachycardia or IST has similar symptoms to Hyperadrenergic POTS. IST patients have a high HR when they are laying down (around 90-100bpm), and slight exertion or emotional stress will cause rapid acceleration. Both conditions can overlap and may have the same underlying causes. Treatment options are similar.
I found an excellent explanation of what adrenergic receptors are at
Dysautonomia International. "Think of adrenergic receptors like a TV antenna (if you are old enough to remember when TVs had antennas!). If the TV antenna picks up a signal, it transmits a message across the screen. In adrenergic receptors, the “signals” are chemicals present in the body called catecholamines (primarily epinephrine and norepinephrine). The “message” is what the catecholamine tells the receptor to do. For example, constrict a blood vessel or make the heart beat faster."
Some people have been found to have auto-antibodies called adrenergic receptor auto=antibodies. So instead of only fighting off a virus or something, their bodies have made auto-antibodies that have attacked and damaged important sites on certain cell membrane proteins and altered their normal cell function. There are two kinds of adrenergic receptor auto-antibodies. One affects the blood pressure and causes it to drop and the other effects the HR and causes it to raise.








 A few months ago I went to the ER and they said I had a urinary tract infection AND shingles. And then more recently, I was in the hospital for bradycardia and low blood pressure, probably orthostatic tachycardia. While I was in there, they said I had another UTI. And then I had a third hospitalization.Needless to say, I am suffering from dehydration and have been pushing fluids.
A few months ago I went to the ER and they said I had a urinary tract infection AND shingles. And then more recently, I was in the hospital for bradycardia and low blood pressure, probably orthostatic tachycardia. While I was in there, they said I had another UTI. And then I had a third hospitalization.Needless to say, I am suffering from dehydration and have been pushing fluids.