Part of the process of being diagnosed with POTS is wondering what caused it and if you did something to cause it and questioning in general.
The list of things that can go wrong in the body and cause POTS is quite extensive. In addition, there are disorders with symptoms like POTS. The secondary disorders are usually treatable and will in turn, treat your POTS symptoms. I would ideally like to make a separate post for each thing. But it will be more efficient to just make links to information within this post.
Adrenal disorders like Addison's disease is one of those conditions that has POTS-like symptoms, meaning that it mimics POTS. If you have an auto-immune disease, you can have an autoimmune type of Addison's disease. And to complicate that further, autoimmune thyroid disease can put you at risk for the autoimmune form of Addison's disease. Other things associated with it are hypoparathyroidism, hypopituitarism, pernicious anemia, testicular failure in men, diabetes type I, and vitiligo.
One of the problems with adrenal glands can be caused by a form of tumor called a Pheochromocytoma. This causes the adrenal glands to be overactive. This can lead to high blood pressure and cause symptoms such as
- Headaches
- Sweating
- Pounding of the heart
- Being shaky
- Being extremely pale
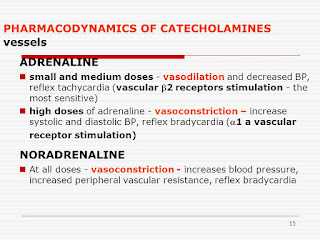
The hormones produced by the adrenal glands belong to a category called Catecholamines, which are released into the bloodstream in response to physical or emotional stress. The ones specific to the adrenal glands are epinephrine and norepinephrine, also called respectively adrenal and noradrenaline. The other catecholamine is dopamine. But it isn't produced by the adrenal glands. Dopamine is produced in the brain. It is a neurohormone that is released by the hypothalamus. Its action is as a hormone that is an inhibitor or prolactin release from the anterior lobe of the pituitary
Pheocychromatoma and paragangliomas cause an overproduction of these hormones. Blood and urine tests to measure the amounts can help detect a pheochromocytoma.
The urine test is a 24-hour urine collection. The blood test for catecholamines is sometimes done when a person has unexplained hypertension or sudden paroxysmal hypertension.
People with Anemia can have symptoms like POTS and if they also have a folic acid deficiency, it will make their anemia and POTS symptoms worse.
Anemia patients sometimes exhibit the symptoms of POTS. Some patients may have a folic acid deficiency, which is contributing to their anemia and POTS symptoms.
Angiotensin II
Some people with POTS have an increased level of Angiotensin II. The renin-angiotensin-aldosterone system (RAAS) helps regulate blood volume by regulating sodium and water retention. Renin and aldosterone can be reduced in POTS patients. But this study found that Angiotensin II was increased. http://www.ncbi.nlm.nih.gov/pubmed/16262605. Angiotensin II is a hormone and it causes blood vessels to constrict.
There may be a gene called the angiotensin II type one receptor gene involved in POTS.
Autoimmune Diseases
Besides anemia and Addison's disease and thyroid disorders, there are several other autoimmune diseases that can cause POTS. See: Lupus, Sjogren's, Guillain-Barre. Sarcoidosis, Crohn's Disease
There is an antibody to neuronal nicotinic acetylcholine receptors of autonomic ganglia that has been discovered. Some POTS patients have higher levels of this antibody. Some patients that also had anhidrosis, constipation, urinary dysfunction, sicca syndrome and pupillary dysfunction had even higher levels. And those that had the highest levels of the antibody, had more severe autonomic dysfunction. And levels of the antibody lower when patients symptoms get better. This indicates cause and effect. Meaning that the antibody can cause POTS and POTS can cause an increase in the level of the antibodies. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671239/
Cardiac Problems
Usually, doctors try to rule out cardiac disease before any diagnosis of POTS.
Problems with the electrical conduction of the heart such as atrioventricular conduction and ventricular repolarization can cause POTS in some patients. Sinus node abnormalities and abnormal P-waves can also cause it. Some patients undergo a procedure called ablation to treat these type of problems. But studies show that the long-term benefits were not good. And it really isn't recommended as a treatment.
In addition, if a patient has been misdiagnosed with sinus tachycardia, it will make their POTS worse to go through ablation. Heart rate-dependent electrocardiogram abnormalities in patients with postural tachycardia syndrome.
Spinal Problems
Cervical stenosis is when there is an area of the spinal canal that is too narrow, and it compresses the spinal cord and nerve roots. Some patients have had craniovertebral decompression which resulted in a decrease or cessation of their POTS symptoms. But other patients did not benefit from it.
Chiari malformation is when the cerebellar tonsils protrude down into the spinal cord. And it can cause the flow of cerebral spinal fluid to be restricted. Some patients have a procedure to correct the Chiari malformation. But not all of them get better afterward. Some doctors think that Chiari malformation causes all POTS, and some do not. Doctors from the NIH and The Chiari Institue say there is a connection between as well as a connection to EDS/Ehlers-Danlos syndrome. There are lots of links here on Chiari malformation and POTS: http://www.dinet.org/index.php/information-resources/pots-place/pots-useful-links
Syringomyelia is a medical condition caused by a cyst growing in the spinal cord. This sometimes causes POTS. Some people also have Chiari malformation. Many POTS patients also report a worsening of symptoms upon straining. One possible explanation of POTS in syringomyelia patients is partial sympathetic denervation of the legs.
Chemicals
Exposure to some chemicals might cause POTS in some patients. Here is a table of some of the possible chemicals: Chemicals and POTS
Ehlers-Danlos Syndrome (EDS), a connective tissue disorder,is found in some POTS patients. Physicians propose that these syndromes occur together due to abnormal connective tissue in dependent blood vessels in those with EDS, which permits veins to distend excessively in response to ordinary hydrostatic pressures (Rowe, Barron, Calkins, Maumenee, Tong & Geraghty, 1999). Simply put, this connective tissue abnormality allows excessive amounts of blood to pool in these patients' lower limbs when they stand up.
There are a variety of types of Ehlers-Danlos syndrome. Classical and type III EDS were originally reported in orthostatic intolerance patients (Rowe et al., 1999). Many POTS patients with EDS have type III (Grubb, 2002).
There can be many symptoms and problems that are associated with the classical and hypermobile types of EDS. Mitral valve prolapse, gastric emptying or motility issues, dilation or rupture of the aorta, hiatal hernia, premature rupture of the membranes during pregnancy, poor wound healing, bruising, joint dislocation, etc.http://ihpotblogspot.blogspot.com/2016/09/joint-hypermobility-syndrome-and-eds.html
Joint Hypermobility Syndrome is a similar disorder. You can read more on them here:
Electrical injury
Electrical injury and being struck by lightning has reportedly occurred prior to the development of POTS in some cases. Lightning strike and autonomic failure -coincidence or causally related?
Liver Disease
A type of liver disease called compensated cirrhosis is when the liver is damaged but is able to compensate for it. This condition causes hypovolemia and vasodilation, POTS and pooling of blood in the lower extremities. Autonomic dysfunction in chronic liver disease
Mast-cell activation disorders
Some people with POTS or other orthostatic intolerance have flushing, palpitations, shortness of breath, chest pain, headache, lightheadedness, hypotension, or hypertension, and syncope
may play a role in the development of POTS in some individuals. Some patients with orthostatic intolerance suffer from episodes of flushing, palpitations, shortness of breath, chest discomfort, headache, lightheadedness, hypotension or hypertension and occasionally syncope, and it is sometimes brought on by an increase in activity. They may also have fatigue, sleepiness, increased urination, and sometimes diarrhea after they have an attack. There are tests for an increase in urinary methylhistamine, which is a marker of mast cell activation, that can be done to find MCAS.
You can read more about MCAS here: A Tale of Two Syndromes – POTS and MCAS
Neuropathy
Some people with neuropathy have POTS. It may be caused by autonomic neuropathy in the cardiovascular system. There may also be sympathetic denervation in the legs. The Neuropathic Postural Tachycardia Syndrome
Nitric Oxide deficit
Nitric Oxide (NO) controls blood vessel size with through changes in blood flow and blood vessels during inflammation and blood vessel leakiness. If you have a deficit of nitric oxide, you may develop POTS. Nitric oxide and regulation of heart rate in patients with postural tachycardia syndrome and healthy subjects
Researchers have found that NO levels can be increased by blocking the most important receptor for angiotensin-II. This may lead to treatments in the future in select groups of POTS patients.
Norepinephrine transporter deficiency
Norepinephrine transporter deficiency causes POTS is some people. These patients have an irregularity in how norepinephrine is used in the body. Under normal conditions, the body recycles norepinephrine. For some people, the protein that causes norepinephrine to be recycled doesn't work properly. And excess norepinephrine is spilled over. They then have depleted levels of norepinephrine if their neurons continue to be stimulated. They go from having excessive amounts of norepinephrine to having no norepinephrine, at which point they crash.Orthostatic Intolerance and Tachycardia Associated with Norepinephrine-Transporter Deficiency
Some patients have hypermethylation of the norepinephrine transporter (NET) gene promoter. When this happens, the gene for the protein that transports norepinephrine (NET) is turned off because its promoter is turned off.
This is a condition is which the left renal vein is congested because it is being compressed by the aorta and the superior mesenteric artery. It may cause a disruption in the renin-angiotensin system. And it also may disrupt the sympathetic adrenal system and overproduction of catecholamines.
Thyroid disease
Thyroid disease can sometimes cause symptoms that are similar to those of POTS.
Tumors
When the body tries to get rid of a tumor by producing antibodies to attack it, sometimes they also attack part of the nervous system. This is called Paraneoplastic Syndrome. This is a rare condition. If the autonomic nervous system is attacked, then the result can be POTS or dysautonomia. Some people get better after the tumor is removed. Some people have to have intravenous immunoglobulin or other immune modulating treatments to try and reduce the harmful antibody levels.
Physical Trauma, Surgery, and Pregnancy
Trauma such as surgery, pregnancy, bariatric surgery, and Traumatic Brain Injury, car accidents, etc. have been shown to precipitate POTS
Viruses
It is estimated that 50% of patients with POTS have a recent history of some sort of virus when they become ill. It has been associated with Epstein-Barr virus. It is believed that viruses may affect the autonomic nervous system directly or that they may cause an autoimmune response that results in POTS.Postural Orthostatic Tachycardia Syndrome (POTS): A Diagnostic Dilemma
Vitamin Deficiencies
People with digestive problems, that are common in people with dysautonomia, frequently have B12 deficiency.
Don't forget to check out the videos at the bottom of the blog. You have to scroll down to the bottom. There is a good one on norepinephrine transporters and one on the sympathetic nervous system.