What is anxiety anyway?
Anxiety is our bodies way of reacting to stress. You have both physical and psychological reactions to stress. People who suffer from anxiety disorders experience excessive fear when there is no real danger and then they begin to avoid the situation that causes it. Anxiety causes disruption in a person's everyday life. It can cause an increased risk for cardiovascular morbidity and mortality in the long run.
But what happens when there are real dangers causing your anxiety? This is what people with chronic illness face every day.
Some examples of these fears are:
- Fear of physical pain. Fear that it's going to continue to worsen or that it will never stop.
- Is my condition permanent? Am I going to die? What is this going to mean for the rest of my life?
- Being afraid of the treatments. Needles, surgeries, tests, they can all be painful and frightening. Fear of medication side effects is pretty prevalent too.
- Fear of not being diagnosed. Some conditions are hard to get an accurate diagnosis for.
Anxiety is believed to start in the amygdala. The amygdala is the area of the brain that controls emotional responses. But it has not been determined if the amygdala is hyper-responsive before the stressor such as symptoms of social phobia, specific phobia, or PTSD appear or if the stressor causes the hyper-responsiveness. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055419/ Neurotransmitters carry the response to the sympathetic nervous system. Then the heart rate and respiration rate increases, and your muscles tense up. And blood flow is diverted from the other organs to the brain. Now due to your anxiety, your body is on high alert. The fight or flight response is in full gear. You may experience nausea, diarrhea, the urge to urinate, light-headedness, pain, headaches, and other physical responses.

According to a Harvard Health article anxiety is associated with many chronic illnesses like heart disease, Chronic Obstructive Pulmonary Disease, and gastrointestinal conditions. If it isn't treated it makes these chronic conditions harder to treat and the patients get worse and their life expectancy is shorter.
It is estimated that about 30% of people suffering from anxiety disorders go untreated. If you suffer from a chronic illness and think you might have it, it is important to discuss it with your primary doctor who can help you find out what is causing your symptoms whether it be physical or psychological. Psychological symptoms are no less real or important than physical ones are. That's what your doctor is there for.
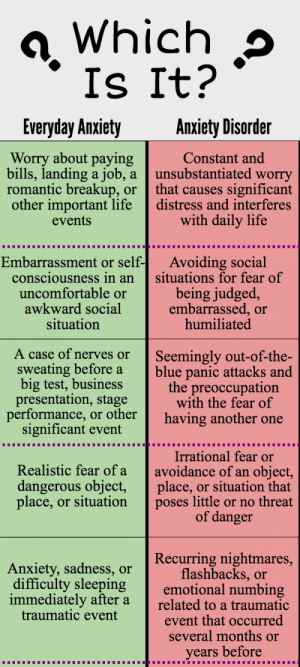
There are several specific types of anxiety disorders.
- Generalized Anxiety Disorder---Patients experience an exaggerated sense of anxiety about health, safety, money, and other aspects of daily life lasting for six months or more. They may also experience headaches, muscle pain, fatigue, nausea, shortness of breath, and insomnia
- Phobias---Patients experience an irrational fear of particular things or situations, such as spiders, being in crowds, or being in enclosed spaces.
- Social Anxiety Disorder--- Patients experience overwhelming self-consciousness in social situations and a feeling of being watched and judged by others and fear of embarrassment.
- Post Traumatic Stress Disorder(PTSD)---Patients relive things from their past that caused an intense physical or emotional threat or an injury such as: childhood abuse, military combat, or an earthquake. They have vivid dreams, flashbacks, or tormented memories. They also experience problems with sleeping or concentrating. They may display angry outbursts, emotional withdrawal, and have a heightened startle response.
- Obsessive Compulsive Disorder--- OCD manifests in obsessive thoughts, that then causes the person to compulsively act in a certain way. An example is having a fear of contamination with germs and then feeling compelled to repeatedly wash your hands in an attempt to lessen the anxiety.
- Panic Disorder---Patients experience episodes of feelings of terror or impending doom, accompanied by rapid heartbeat, sweating, dizziness, or weakness with no apparent provocation.

:max_bytes(150000):strip_icc()/social-anxiety-disorder-causes-3024749-5c3b8f7bc9e77c0001bffa28.png)
These problems can cause complications in chronic illness. For instance, studies have shown that patients that have COPD have high rates of anxiety and panic attacks. This, in turn, causes higher incidents of hospitalization and severe respiratory distress. When you can't catch your breath, anxiety, and panic are pretty understandable. And it would obviously adversely affect your quality of life. Managing Panic Attacks When You Have COPD
The development of heart disease and resultant coronary events have been linked to anxiety disorders. Women with high levels of anxiety were 59% more likely to have a heart attack and 31% more likely to die from it than women with low anxiety in the Nurses Health Study.
A study done at Harvard Medical School and one done at the Lown Cardiovascular Research Institute showed that people with heart disease who also had an anxiety disorder were 2 times more likely to have a heart attack than other people. Anxiety and heart disease: A complex connection

There are treatments for anxiety disorders and they can help treat chronic illnesses and even help prevent heart disease and treat existing heart disease. But treatments need to be tailored to the individual patient. https://www.anxiety.org/treatments
- Cognitive-behavioral therapy. This works by helping the patient identify and avoid thoughts that cause anxiety, and then helps them learn how to react differently to anxiety-provoking situations. It has to be tailored to the patients particular type of anxiety. Patients may learn relaxation techniques to lessen their anxiety.
- Psychodynamic psychotherapy. When anxiety is caused by an emotional trauma it the patient can sometimes benefit from therapy. Research at Colombia University showed that patients suffering from a panic disorder who were treated with psychotherapy had fewer symptoms and were able to function socially better than patients who were treated with relaxation therapy.
There is a tendency for patients and doctors alike to rely mainly on medications to treat anxiety. But on their own, medications don't work as well as when they are combined with psychotherapy. Many of them come with side effects. But they are useful to get the patients symptoms under control so that therapy can be more effective.
These medications consist of anti-anxiety drugs like benzodiazepines(Klonipin, Xanax) There is a newer drug called Buspar that is supposed to have fewer side effects. Whereas the others work quickly, Buspar takes about two weeks to kick in. But it can be taken for longer periods of time than the others.
Antidepressants like Zoloft which is a selective serotonin reuptake inhibitor (SSRI) are used to treat panic disorder and generalized anxiety disorder (GAD). They also treat depression. They are considered to have a lower risk of drug dependence or abuse.
Beta blockers are used to treat anxiety by slowing the heart rate and reducing blood pressure.
DEPRESSION
Depression can occur independent of or in relation to anxiety and may have overlapping symptoms. It is common for people with chronic illnesses to suffer from depression. It makes their conditions harder to treat and can make it worse. If patients are treated for depression it can lessen their stress and result in an improvement of their symptoms, resulting in increased quality of life.The World Health Organization (WHO) says that depression is the leading cause of disability in the world and the 4th leading cause of the global burden of disease. They estimate that by 2020, depression will be the 2nd public health concern next to cardiovascular disease. https://www.who.int/news-room/fact-sheets/detail/depression

The criteria for depression in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), major depressive disorder (MDD) the most severe form of depression, is an episode that lasts at least 2 weeks with the patient having at least 5 out of 9 depressive symptoms. One of the symptoms has to be depressed mood or loss of interest or pleasure in anything (anhedonia). Symptoms have to cause significant distress and social, occupational impairment or impairment in other areas of their lives resulting in noticeable disability caused by their illness.
Symptoms of depression are:
- Feeling sad, irritable, or anxious
- Feeling empty, hopeless, guilty, or worthless
- Loss of pleasure in usually-enjoyed hobbies or activities, including sex
- Fatigue and decreased energy, feeling listless
- Trouble concentrating, remembering details, and making decisions
- Not being able to sleep, or sleeping too much. Waking too early
- Eating too much or not wanting to eat at all, possibly with unplanned weight gain or loss
- Thoughts of death, suicide or suicide attempts
- Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment
People with chronic illness have some of the same risk factors for depression as people in the general population. Things like a personal or family history of depression or loss of family members to suicide are risk factors for depression.
There are some conditions that are themselves risk factors for depression due to causing changes within the brain, such as, Parkinson’s Disease and strokes.
Depression is common among people who have chronic illnesses such as the following:
- Cancer
- Coronary heart disease
- Diabetes
- Epilepsy(Mood, Anxiety and Depression | Advice From Epilepsy Society)
- Multiple sclerosis
- Stroke
- Alzheimer’s disease
- HIV/AIDS
- Parkinson’s disease(Parkinson's disease and anxiety: comorbidity with depression)
- Systemic lupus erythematosus(Lupus and depression: Know the signs and how to get help )
- Sjogren's Syndrome (Anxiety and depression in primary Sjögren's syndrome)
- Rheumatoid arthritis(Rheumatoid Arthritis Linked To Serious Mood Disorders)
- Fibromyalgia(Fibromyalgia and Depression: Effects, Treatments, Signs, and More)
- Crohn's Disease(Signs and Symptoms of Depression | Crohn's & Colitis Foundation)
There are many others.
The rate of anxiety and depression depends on the type and severity of the chronic illness is. But the rates are higher across the board among people with chronic illness in comparison to the general population. It is particularly prevalent in stroke, cardiovascular and diabetic patients.
This is an interesting article about people with the autoimmune condition Sjogren's Syndrome and how they differ from the general population. Sjögren’s Patients Exhibit Different Personality Traits than Healthy Individuals, Study Suggests
Studies suggest that people who have depression and another medical illness experience more severe symptoms of both their depression and their physical illnesses. They can have difficulty adapting to both and higher medical expenses than patients who do not suffer from depression.
People who have been diagnosed with a chronic illness often feel sadness because of the major changes in their lives due to the disease like fatigue and other physical limitations that make their normal activities harder or impossible. They may also feel frustration. Patients often feel anxiety because of uncertainty about what the future holds and the prognosis of their disease because it may be incurable or unpredictable and precarious. And the fear of death can cause great depression and anxiety. They may experience sleep disturbances as a result. If they are able to regain some of their normal functions and participate in their regular daily life their symptoms were reduced.
Chronic illness causes people to be isolated socially due to less contact with friends and family because they can't get out as much. Their friends may also avoid them because they don't know how to deal with their friend's conditions and they may feel like they no longer have anything to relate to.
If you have symptoms like shortness of breath, panic attacks, sensitivity to noise, brain fog, etc. it may cause anxiety and other symptoms that may cause you to remain home further exacerbating your social isolation.
People with chronic illness often express feelings of guilt which makes their anxiety and depression worse. They feel like they are the blame for getting their conditions. Perhaps they didn't take as good of care of themselves as they feel they should have. They also feel shame because they find it difficult to be grateful for being alive.
Another aspect of anxiety and depression in chronic illness is that doctors tend to feel like it is just a normal part of the disease and downplay its importance or in contrast, they might chalk of many of the patient's physical symptoms to their depression causing the patient to rightfully feel dismissed. But to be fair to physicians, the physical symptoms of chronic diseases overlap with depression and anxiety and this makes diagnosis difficult. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3817854/
The condition known as POTS, Postural Orthostatic Tachycardia is complicated when it comes to anxiety and depression. Postural Orthostatic Tachycardia Syndrome (POTS) is a condition in which heart rate increases abnormally when the individual assumes an upright position. In addition to the marked tachycardia, presyncope, and syncope. Considering the marked elevation in heart rate on standing, increased anxiety about this and the feeling of faintness or actual syncope is not surprising. But many doctors are prone to completely dismissing the condition as just anxiety. This Mysterious Blood-Flow Disorder Is Often Misdiagnosed As Depression
One study in the United Kingdom found that nearly 50 percent of POTS patients had previously been told they had a psychiatric disorder that was responsible for their symptoms.
Cognitive function, health-related quality of life, and symptoms of depression and anxiety sensitivity are impaired in patients with the postural orthostatic tachycardia syndrome (POTS)
In a Vanderbilt University study, Patients with POTS had a markedly diminished quality of life in both physical health and mental/social health domains compared to the healthy volunteers. The scores were comparable to previously published scores for patients with kidney failure requiring hemodialysis. The Vanderbilt data were similar to a prior publication from the Mayo Clinic {PMID: 12059122} that also found diminished quality of life in patients with POTS. https://ww2.mc.vanderbilt.edu/adc/43572
What does anxiety have to do with PoTS?
Research has shown that PoTS is not the same as anxiety. However, PoTS is sometimes confused with anxiety because:
- Anxiety is so common that, just by chance, many people with PoTS will also have anxiety.
- Some of the symptoms of anxiety are similar to the symptoms of PoTS. Palpitations, nausea, light-headedness, gut symptoms, fatigue, and headaches are symptoms that can occur both in anxiety and as a result of PoTS.
- Even when we know that PoTS symptoms are not harmful, symptoms can still feel very frightening. Adding scary thoughts to the mix can increase symptoms even more.
- Worrying excessively about a thing that could happen in the future can lead to low moods. It can help to recognize that these problems have not yet happened and may never happen. Deal with problems as they come up, and use your time and energy on more positive thoughts.
- Anxiety and stress cause our bodies to release a chemical in the blood stream called norepinephrine. People with PoTS seem to be very sensitive to this chemical which can cause symptoms like anxiety. In addition, the parasympathetic nervous system which calms us, may also not be functioning normally in PoTS.
I have shown that people with chronic illnesses are more likely to have anxiety and depression. But people who are depressed are also more likely to have chronic illnesses like cardiovascular disease, diabetes, stroke, and Alzheimer’s disease.
Scientists have found that people who suffer from depression show changes in several different systems in the body:
- Signs of increased inflammation
- Changes in the control of heart rate and blood circulation
- Abnormalities in stress hormones
- Metabolic changes typical of those seen in people at risk for diabetes
Even though you and your doctors may be tempted to dismiss depression and anxiety as a normal part of your illness, DON'T. Treatment for depression is available and can help even if you have another chronic illness or condition. If you think you or a loved one have depression, it is vitally important to tell your doctor so they can help you find treatment options.
It may take some time to recover from depression but being treated can help improve your quality of life.
You Can Find More Information With The Following:
https://adaa.org/understanding-anxiety
https://www.verywellmind.com/social-anxiety-disorder-causes-3024749
https://www.healthline.com/health/anxiety/effects-on-body#1
https://www.anxietycentre.com/anxiety-symptoms.shtml
National Institute of Mental Health http://www.nimh.nih.gov/health/topics/depression/index.shtml
En Español http://www.nimh.nih.gov/health/publications/espanol/depresion/index.shtml
For more information on conditions that affect mental health, resources, and research, go to MentalHealth.gov at http://www.mentalhealth.gov, or the NIMH website at http://www.nimh.nih.gov. In addition, the National Library of Medicine’s MedlinePlus service has information on a wide variety of health topics, including conditions that affect mental health.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
Science Writing, Press, and Dissemination Branch
6001 Executive Boulevard
Room 6200, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513 or 1-866-615-NIMH (6464) toll-free
TTY: 301-443-8431 or 1-866-415-8051 toll-free
Fax: 301-443-4279
Email: nimhinfo@nih.gov
Website: http://www.nimh.nih.gov







